The NMC OSCE NEWS2 chart (National Early Warning Score 2) is a standardised clinical assessment tool you’ll use in the NMC OSCE exam to monitor patient deterioration and guide escalation decisions. You must accurately record six vital signs (respiration rate, oxygen saturation, systolic blood pressure, pulse rate, consciousness level, and temperature), calculate the total score correctly, and escalate appropriately based on evidence-based protocols. Mastering the NMC OSCE NEWS2 chart demonstrates safe clinical reasoning – a core 2026 NMC competency – and is non-negotiable for passing your Assessment Station and delivering safe patient care as a UK registered nurse. Understanding the NMC OSCE NEWS2 chart is vital for success in your nursing career.
Table of Contents
Why the NEWS2 Chart Matters: Your Bridge to Safe Practice and Clinical Reasoning
You’ve just finished gathering vital signs during your OSCE Assessment Station. The patient’s respiratory rate is 24, oxygen saturation 94%, blood pressure 148/92, pulse 102, temperature 38.5°C, and they’re alert. Now what?
This is where many nurses freeze. They have the observations, but they don’t know how to interpret them clinically or escalate appropriately. In the 2026 NMC framework, this gap between collecting data and acting on data-between procedure and clinical reasoning-is the difference between passing and failing.
The NEWS2 chart isn’t just bureaucratic paperwork. It’s a clinical reasoning tool that prevents missed deterioration and saves lives. In UK hospitals, NEWS2 underpins the entire patient safety infrastructure. Getting it right in your OSCE exam directly translates to delivering safe, person-centred care as a registered nurse.
Based on our experience training 1500+ international nurses for UK OSCE, we’ve identified that NEWS2 mastery involves three critical layers:
- Technical accuracy – Recording vital signs correctly
- Scoring precision – Applying the NEWS2 algorithm without error
- Clinical interpretation – Understanding what the numbers mean and why escalation matters
This guide walks you through all three layers-starting with what the six vital signs mean, progressing to step-by-step scoring, and culminating in real OSCE scenarios. You’ll also see the common mistakes that cost candidates marks and exact strategies to avoid them.

Understanding NEWS2: The Six Vital Sign Components and Why Each Matters
Before you can score NEWS2, you need to understand what you’re measuring and why each vital sign matters clinically. This is the foundation of 2026 NMC clinical reasoning expectations.
The Six Physiological Parameters You’ll Assess
The NEWS2 chart assesses exactly six vital signs. Each tells a story about patient deterioration:
1. Respiration Rate (Breaths Per Minute)
- Normal range: 12-20 breaths/minute
- Why it matters: Respiratory rate reflects oxygenation, acid-base balance, and pain/anxiety levels. A rising RR often signals deterioration before other vital signs change.
- What examiners watch for:
- Are you counting for a full 60 seconds without the patient knowing?
- Do you notice laboured or shallow breathing?
- Can you differentiate between normal and distressed breathing?
- Can you link RR changes to clinical context (e.g., infection, pain, pulmonary embolism)?
Examiner insight (2026): You’re not just counting breaths. You’re assessing respiratory effort. Examiners listen for: “The patient has a respiratory rate of 26, which is elevated. Additionally, I notice they’re using accessory muscles and their breathing appears laboured, suggesting possible respiratory distress.”
2. Oxygen Saturation (SpO₂as a Percentage)
- Normal range: 95-100%
- Critical clinical note: SpO₂ targets vary by patient condition. A COPD patient’s target SpO₂ might be 88-92%, not 95-100%.
- What examiners watch for:
- Correct placement of the pulse oximetry probe
- Recognition that SpO₂ on oxygen versus on room air changes interpretation
- Understanding of hypoxaemia as a red flag
- Ability to explain why a low reading is concerning (e.g., “SpO₂ 91% could indicate pneumonia or pulmonary embolism”)
Examiner insight (2026): Context is everything. Don’t just report numbers. Say: “Patient’s SpO₂ is 92% on 28% oxygen delivered via nasal cannula. For a COPD patient, this is within their target range, but I would monitor for further deterioration. If SpO₂ drops below 88%, I would escalate.”
3. Systolic Blood Pressure (Top Number Only)
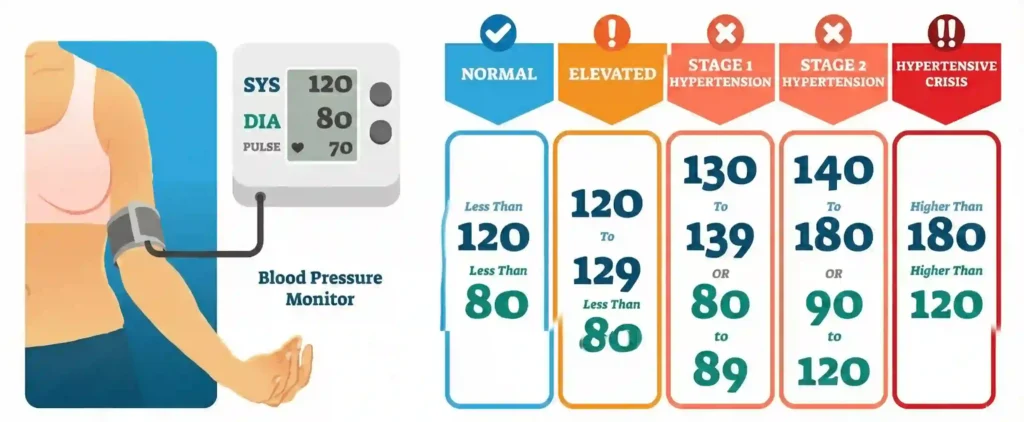
- Normal: Less than 120/80 mmHg
- Elevated: Systolic 120–129 mmHg and diastolic < 80 mmHg
- Stage 1 Hypertension: Systolic 130–139 mmHg or diastolic 80–89 mmHg
- Stage 2 Hypertension: Systolic 140–180 mmHg or diastolic 90–120 mmHg
- Hypertensive Crisis: Systolic > 180 mmHg and/or diastolic > 120 mmHg (medical emergency)
What examiners watch for:
- Accurate blood pressure measurement using an upper-arm cuff
- Correct cuff placement and appropriate cuff size
- Proper patient positioning (arm supported at heart level)
- Correct identification and classification of abnormal readings
- Prompt reporting and escalation of significantly high or low values
Examiner insight (2026): Examiners may ask, “This patient’s BP is 88/54. What are you concerned about?” The answer shows clinical reasoning: “Systolic BP 88 indicates hypotension. Combined with tachycardia and fever, this could suggest sepsis or hypovolaemic shock. I would escalate immediately.”
4. Pulse Rate (Beats Per Minute)
- Normal range: 51-100 beats/minute
- What examiners watch for:
- Full 60-second count (or 15 seconds × 4 in time-pressed situations, but 60 is preferred)
- Ability to detect irregularities (arrhythmias, atrial fibrillation)
- Recognition that tachycardia can indicate infection, pain, anxiety, or decompensation
- Understanding that bradycardia (< 50) can indicate cardiac problems or medication effects
Examiner insight (2026): Don’t just report the number. Assess rhythm: “Pulse is 106 and regular. The elevation could be due to fever and infection rather than a primary cardiac issue, but I would continue to monitor.”
5. Level of Consciousness (AVPU Scale)
Disability:Assess the patient’s conscious level using AVPU (Alert, Voice, Pain, Unresponsive).
Also consider confusion, response to pain, urine output, and blood glucose, as these can influence or explain changes in consciousness.
AVPU explained:
- A = Alert–fully conscious, orientated
- V = Verbal–responds to voice
- P = Pain–responds only to pain stimulus
- U = Unresponsive–no response to any stimulus
Why it matters
Level of consciousness is a critical indicator of brain perfusion and neurological deterioration.
Any change in consciousness, especially reduced consciousness, is always an emergency.
What examiners watch for
- Systematic assessment
- Ask questions first
- Then use voice
- Then apply pain stimulus
- Recognition of deterioration
- A patient becoming “drowsy”from “alert”is a red flag
- Understanding of assessment tools
- Glasgow Coma Scale (GCS) is more detailed
- AVPU is used in NEWS2
Examiner Insight (2026)
Examiners expect you to identify and clearly state changes.
If a patient was alert on admission but is now responding only to voice, say:
“The patient’s level of consciousness has changed from Alert to Verbal. This is concerning for deterioration and requires urgent escalation.”
6. Temperature (in Degrees Celsius)
- Normal range: 36.5-37.5°C
- What examiners watch for:
- Correct thermometer use (non-contact temporal or digital preferred in modern practice)
- Recognition that fever (> 38°C) is a red flag for infection
- Understanding that hypothermia (< 36°C) can indicate sepsis or other serious conditions
- Ability to link temperature to other vital signs (fever + tachycardia + tachypnoea = possible infection)
Examiner insight (2026): Context matters. A post-operative patient with fever day 1 post-op may be normal. A patient with fever + cough + tachypnoea suggests pneumonia. Your job is to recognise the pattern.
How NEWS2 Scoring Works: The Point System Explained
Each of the six vital signs is assigned a score from 0 to 3 based on how far it deviates from normal values:
- Score 0 = Normal (no concern)
- Score 1 = Slightly abnormal (monitor closely) 1 ALSO REQUIRED ESCALATION
- Score 2 = Moderately abnormal (escalate)
- Score 3 = Severely abnormal (urgent escalation required)
The total NEWS2 score is the sum of all six individual scores, ranging from 0 to 18. Here’s the complete scoring reference table:
| Vital Sign | Score 0 | Score 1 | Score 2 | Score 3 |
| Respiration Rate (breaths/min) | 12-20 | 9-11 or 21-24 | 25-30 | <9 or >30 |
| SpO₂ (%) | 95-100 | 93-94 | 91-92 | <91 |
| Systolic BP (mmHg) | 90-180 | 81-89 or 181-200 | 71-80 or 201-220 | <71 or >220 |
| Pulse Rate (beats/min) | 51-100 | 41-50 or 101-110 | 111-130 | <41 or >130 |
| Consciousness (AVPU) | Alert | – | Verbal or Pain | Unresponsive |
| Temperature (°C) | 36.5-37.5 | 35.1-36.4 or 37.6-38.4 | 38.5-39 | <35.1 or >39 |
Worked Example: A patient has:
- Respiration rate 26 → Score 2 (range 25-30)
- SpO₂ 94% → Score 1 (range 93-94)
- Systolic BP 175 → Score 0 (range 90-180)
- Pulse 108 → Score 1 (range 101-110)
- Consciousness: Alert → Score 0
- Temperature 37.2°C → Score 0 (range 36.5-37.5)
- Total NEWS2 = 2 + 1 + 0 + 1 + 0 + 0 = 4
This patient would require escalation to the nurse-in-charge and increased monitoring (4-6 hourly).
Recording Observations on the NEWS2 Chart: The Exact Step-by-Step Process Examiners Expect
Filling out NEWS2 accurately is non-negotiable. This is where technical precision meets clinical awareness. Here’s the exact process examiners watch for:
Step 1: Read the Patient Scenario Carefully (Contextual Foundation)
Before you even touch a thermometer, understand the clinical picture:
- Who is this patient? (Age, gender, occupation can influence baseline vital signs)
- What is their presenting problem? (Infection? Respiratory distress? Cardiac event?)
- Are they on oxygen? (If yes, what is the delivery method and FiO₂?)
- Do they have chronic conditions? (COPD, diabetes, heart failure-these affect interpretation)
- What is their baseline? (Post-operative patients may have elevated RR and pulse normally)
Example scenario: “Mrs Khan is a 72-year-old admitted with community-acquired pneumonia. She has a history of COPD and is on oxygen 28% via nasal cannula. She lives independently at home with her husband.”
This context shapes everything. For Mrs Khan:
- An SpO₂ of 92% on her oxygen is acceptable (not an emergency)
- An elevated RR of 24 is expected with pneumonia (but combined with fever, this suggests active infection)
- Tachycardia is expected during infection
2026 NMC Context: Examiners in 2026 expect you to demonstrate clinical reasoning before you record numbers. Verbalise your thinking: “Mrs Khan has pneumonia, so I expect elevated respiratory rate and heart rate as signs of infection fighting. However, I need to monitor for deterioration indicators.”
Step 2: Take Each Vital Sign Using Correct Technique
Respiration Rate: Full 60-Second Observation
- Position yourself so the patient doesn’t know you’re observing (patients change breathing when aware)
- Observe the rise and fall of the chest
- Count for a full 60 seconds (not 30 seconds × 2)
- Note the quality of breathing: shallow or deep? Laboured or easy? Using accessory muscles?
- Record the number
Examiner watch: An examiner will observe your counting technique. Count silently and steadily. Don’t tap your fingers or move your lips.
Oxygen Saturation: Proper Probe Placement
- Ensure the pulse oximetry probe is placed correctly (typically on the fingertip or earlobe)
- Remove any nail polish (can give false readings)
- Wait for the reading to stabilise (2-3 seconds)
- Note the oxygen delivery method (room air? 2 litres nasal cannula? Non-rebreather mask?)
- Record the SpO₂ percentage and oxygen source
Examiner watch: Say aloud, “Patient’s SpO₂ is 96% on room air,” so the examiner hears that you’re considering context.
Systolic Blood Pressure: Cuff and Positioning
- Select the correct cuff size (too small = high reading; too large = low reading)
- Position patient seated or semi-recumbent with arm at heart level
- Inflate the cuff smoothly to about 20 mmHg above the point where you lose the pulse
- Slowly deflate and note the systolic pressure (when you first hear Korotkoff sounds)
- Record only the systolic (top) number
Examiner watch: Examiners assess your attention to detail. Correct cuff size, proper positioning, and accurate reading all matter.
Pulse Rate: Full Palpation Count
- Locate the pulse (radial is most common; carotid or femoral if radial absent)
- Palpate gently with two fingers (index and middle)
- Count for a full 60 seconds
- Assess rhythm (regular or irregular?)
- Note any quality issues (weak, bounding, irregular)
Examiner watch: If the pulse is irregular (e.g., atrial fibrillation), flag this. Say, “Patient’s pulse is irregular at 102 beats per minute, which could indicate arrhythmia. I would escalate for ECG assessment.”
Level of Consciousness: Systematic AVPU Assessment
- Start with conversation: Is the patient alert and orientated? Can they tell you their name, date, and location?
- If no response, use voice: Call their name loudly. Do they open their eyes or respond?
- If still no response, apply pain stimulus: Press on the sternum or trapezius. Do they respond to pain?
- Determine the level: Alert (A), Verbal (V), Pain (P), or Unresponsive (U)
Examiner watch: Examiners will watch your assessment method carefully. Be systematic and thorough.
Temperature: Non-Contact or Digital Thermometer
- Use a non-contact (temporal) thermometer for speed and infection control
- Or use a digital thermometer (axillary, oral, or tympanic)
- Avoid mercury thermometers (outdated and hazardous)
- Wait for the reading to stabilise
- Record in Celsius
Examiner watch: Know the normal range (36.5-37.5°C) so you can immediately flag fever or hypothermia.
Step 3: Assign the Correct NEWS2 Score for Each Parameter
For each vital sign, compare your recorded value to the NEWS2 scoring table and assign 0, 1, 2, or 3.
Worked Example-Patient Vitals:
- Respiration rate: 22 breaths/min → Score 1 (range 21-24)
- SpO₂: 96% → Score 0 (range 95-100)
- Systolic BP: 165 mmHg → Score 0 (range 90-180)
- Pulse: 92 bpm → Score 0 (range 51-100)
- Consciousness: Alert → Score 0 (Alert is always 0)
- Temperature: 37.8°C → Score 1 (range 37.6-38.4)
Subtotal: 1 + 0 + 0 + 0 + 0 + 1 = 2
Tip for accuracy: Use the scoring table every time. Don’t try to memorise ranges-reference the table to ensure precision.
Step 4: Calculate the Total NEWS2 Score
Sum all six individual scores. This total (ranging 0-18) determines your escalation response.
Critical Rule-The “Score 3 Anywhere” Rule:
Even if the total score is low, if ANY single parameter scores 3, you must escalate immediately. This is a safety rule that overrides the total.
Example: A patient has NEWS2 total of 3, but consciousness level = Unresponsive (Score 3). Despite the low total, this is an emergency requiring immediate escalation.
Step 5: Identify the Escalation Pathway and Monitoring Frequency
Based on your total NEWS2 score, identify the appropriate clinical action and monitoring frequency:
| Total NEWS2 Score | Clinical Action | Monitoring Frequency |
| 0 | Continue routine monitoring | 12-hourly |
| 1-4 | Inform nurse-in-charge; increase observations as needed | 4-6 hourly |
| 3 in any one parameter | Urgent review by registered nurse or clinician | Hourly until stable |
| 5-6 | Urgent response: Inform senior nurse/medical team; consider critical care referral | Hourly |
| ≥7 | Emergency response: Immediate senior clinician review; critical care involvement | Continuous monitoring |
In your OSCE exam, you’ll circle or highlight the appropriate row on the printed chart.
2026 NMC Expectation: Don’t just circle a box silently. Examiners expect you to explain why you’re escalating. Say: “Patient’s total NEWS2 is 5, which indicates urgent escalation to the medical team. This combined score of 5 places them in the orange zone, requiring urgent senior review and hourly monitoring to detect further deterioration.”
Interpreting NEWS2 Scores: Moving Beyond Numbers to Clinical Reasoning
Understanding the clinical significance behind the numbers is what separates nurses who pass OSCE from those who fail. This is the heart of 2026 NMC clinical reasoning expectations.
NEWS2 Score 0: Green Light (Routine Monitoring)
Clinical meaning: Patient is stable. All vital signs within normal range. No acute concerns.
Your response:
- Continue routine observations (12-hourly)
- Document clearly
- Inform patient they’re doing well
- No escalation needed
OSCE expectation: State confidently: “Patient’s observations are all within normal limits. Total NEWS2 is 0. This patient is stable. I would continue routine monitoring and ensure they’re comfortable.”
Example scenario: Pre-operative patient with all normal vital signs before elective surgery.
NEWS2 Score 1-4: Amber Light (Increased Surveillance Required)
Clinical meaning: Patient has some abnormalities, but not yet critical. Close monitoring required to catch deterioration early.
Your response:
- Increase observation frequency to 4-6 hourly
- Inform the nurse-in-charge
- Assess whether additional clinical review is needed
- Watch for patterns (fever + cough + tachypnoea = possible pneumonia)
- Reassess if patient develops new symptoms
OSCE expectation: Verbalise thoughtfully: “Patient’s NEWS2 is 3. They have slightly elevated respiratory rate and mild fever, suggesting possible early infection. I would increase observations to 4-6 hourly and inform the nurse-in-charge. If fever or respiratory rate increases further, I would escalate to the medical team.”
Example scenario: Patient admitted with minor urinary tract infection. Mild fever, elevated RR, otherwise stable.
NEWS2 Score 5-6 OR Any Parameter Scoring 3: Orange Light (Urgent Escalation)
Clinical meaning: Red flags are present. Deterioration is evident. Senior clinical review required immediately.
Your response:
- Call for urgent assessment by registered nurse, doctor, or senior clinician
- Increase monitoring to hourly
- Document the concern clearly and completely
- Prepare for possible transfer to higher level of care
- Stay alert for further deterioration
OSCE expectation: Demonstrate clinical reasoning and urgency: “Patient’s NEWS2 is 6. Specifically, they have elevated respiratory rate (28), lower SpO₂ (91%), and tachycardia (106). Combined with fever (38.5°C), this pattern suggests possible infection, possibly pneumonia or urinary sepsis. I would immediately escalate to the medical team for urgent assessment and possible investigations including blood cultures and chest X-ray.”
Example scenario: Post-operative patient day 2 with fever, tachycardia, tachypnoea-possible surgical site infection or sepsis developing.
NEWS2 Score ≥7: Red Light (Medical Emergency)
Clinical meaning: Patient is critically unwell. Immediate intervention required. Time is critical.
Your response:
- This is a medical emergency
- Activate the emergency response (call for senior clinician immediately)
- Implement continuous monitoring
- Prepare for ICU admission
- Consider what immediate interventions might be needed (IV access, oxygen escalation, fluid resuscitation for shock)
- Keep the patient’s family informed
OSCE expectation: Demonstrate urgency without panic: “Patient’s NEWS2 is 8. This is a medical emergency. Multiple red flags present: high fever (39.2°C), tachycardia (118), tachypnoea (28), low SpO₂ (89%), and borderline hypotension (88/54). This pattern is highly concerning for sepsis. I would immediately alert the medical team and prepare for critical care escalation. I would also ensure continuous monitoring is in place and establish IV access if not already present.”
Example scenario: Patient deteriorating with signs of septic shock (fever, tachycardia, hypotension, altered mental status).
Common Mistakes Nurses Make in NEWS2 Scoring (And How to Fix Them)
After training hundreds of nurses, we’ve identified the recurring errors that cost candidates marks. Here’s how to avoid them:
Mistake 1: Forgetting the “Score 3 Anywhere” Rule
What happens: Candidate records a patient with consciousness = Unresponsive (Score 3), but total NEWS2 is only 2. They say, “No escalation needed.”
Why it fails: An unresponsive patient is critically unwell, regardless of other vital signs. Missing this rule shows poor clinical judgment.
How to fix: MEMORISE this rule: Any single parameter scoring 3 = automatic urgent escalation, even if total score is low. In OSCE, explicitly state this awareness: “Patient has a score of 3 in consciousness level (unresponsive). Even though my total NEWS2 is 2, I would escalate urgently for emergency assessment because consciousness level scoring 3 is always a medical emergency.”
Mistake 2: Temperature Range Confusion
What happens: Patient has temperature 38.4°C. Candidate scores it as 2 instead of 1.
Why it fails: Inaccurate scoring leads to incorrect escalation decisions.
How to fix: Memorise these exact boundaries:
- 36.5-37.5°C = Score 0
- 35.1-36.4 or 37.6-38.4 = Score 1
- 38.5-39°C = Score 2
- <35.1 or >39°C = Score 3
Memory trick: Think of 37.6 and 38.4 as the boundaries for Score 1. Temperature 38.4 is still in the Score 1 range. Temperature 38.5 steps up to Score 2.
Mistake 3: Ignoring SpO₂Context (Especially COPD Patients)
What happens: A COPD patient has SpO₂ 89%. Candidate immediately escalates as emergency. Examiner asks, “This patient has COPD. What are you concerned about?”
Why it fails: The candidate didn’t recognise that SpO₂ targets vary by condition. Some COPD patients safely maintain 88-92% SpO₂.
How to fix: Always acknowledge context: “Patient has COPD with a target SpO₂ of 88-92%. Current reading of 89% is acceptable for her condition. However, I would monitor for any further deterioration. If SpO₂ drops below 88% or patient develops respiratory distress, I would escalate.” This shows clinical reasoning, not just algorithmic scoring.
Mistake 4: Failing to Escalate When NEWS2 ≥5
What happens: Candidate correctly calculates NEWS2 = 6 but says, “I would monitor and see if it improves.” No escalation mentioned.
Why it fails: Delaying escalation of NEWS2 ≥5 is unsafe practice. This is a major mark loss demonstrating poor clinical judgment.
How to fix: The moment you calculate NEWS2 ≥5, immediately state: “I would escalate this to the medical team urgently.” Don’t hesitate. Don’t suggest waiting. Escalate immediately.
Mistake 5: Blood Pressure Range Errors
What happens: Patient BP is 88/55. Candidate scores systolic as 1 instead of 2.
Why it fails: Hypotension (80-89) indicates possible shock and requires urgent assessment.
How to fix: Memorise these BP systolic boundaries:
- 90-180 = Score 0
- 81-89 or 181-200 = Score 1
- 71-80 or 201-220 = Score 2
- <71 or >220 = Score 3
A BP of 88 = Score 1. A BP of 75 = Score 2. Know the ranges.
Mistake 6: Inaccurate Respiratory Rate Counting
What happens: Examiner watches you count RR. You count for only 30 seconds and multiply by 2. Or you count too quickly and miss a breath.
Why it fails: RR is a key indicator of respiratory distress. Inaccurate counting = inaccurate escalation decisions.
How to fix: Always count for a full 60 seconds. If time-pressed, 60 seconds of accuracy beats 30 seconds of speed. Also, observe before the patient knows you’re counting (patients change breathing when aware).
Mistake 7: Missing Changes in Consciousness
What happens: Patient has NEWS2 = 2, but consciousness has dropped from Alert to Verbal. Candidate doesn’t flag this.
Why it fails: A change in consciousness is an emergency, even if overall NEWS2 is low.
How to fix: Always note if consciousness has changed. A patient who was alert but is now drowsy needs urgent review. Examiners expect you to flag this: “Although vital signs are relatively stable, patient’s consciousness has changed from alert to drowsy. This deterioration warrants urgent medical review.”
Mistake 8: Not Explaining Your Escalation
What happens: Candidate circles the escalation box on the chart but doesn’t explain why.
Why it fails: 2026 NMC standards expect clinical reasoning. Just circling a box shows procedure, not thinking.
How to fix: Always explain: “Patient’s NEWS2 is 5. The concerning features are elevated respiratory rate (26), lower SpO₂ (92%), and fever (38.7°C). This pattern suggests possible respiratory infection. I would escalate to the medical team for urgent assessment and investigations.”
Mistake 9: Documenting Poorly or Incompletely
What happens: Candidate records vital signs but doesn’t document escalation action or patient education.
Why it fails: Poor documentation suggests poor practice. Examiners expect complete, clear, professional records.
How to fix: Document:
- Time of observations- DATE ALSO NEED TO DOCUMENT
- Each vital sign recorded
- NEWS2 score calculated
- Escalation action taken (or reason no escalation)
- Patient communication (what you explained to them)
- Next steps (e.g., “Awaiting medical team assessment”)
Mistake 10: Panic When Scores Seem High
What happens: Candidate calculates NEWS2 = 7 and freezes or becomes flustered.
Why it fails: Panic leads to errors. Examiners watch for composure and clinical competence.
How to fix: Stay calm. Recheck your scoring. Escalate appropriately. Take a breath and follow the protocol. Say aloud: “Total NEWS2 is 7. This is a medical emergency. I’m immediately alerting the medical team.”
The 2026 NMC Framework: How NEWS2 Fits Into Updated Competency Standards
The 2026 NMC competency updates have fundamentally shifted OSCE assessment away from pure procedural accuracy and toward integrated clinical reasoning. Understanding this shift is critical to passing your exam.
Shift 1: From Data Collection to Data Interpretation
Old approach (pre-2026): Record vital signs accurately. Calculate NEWS2. Done.
New approach (2026+): Record vital signs. Calculate NEWS2. Explain what the pattern means clinically and why escalation is necessary.
In your OSCE exam, don’t just report numbers. Demonstrate clinical reasoning. Instead of: “NEWS2 is 5,” say: “Patient’s NEWS2 is 5. The pattern shows fever (38.8°C), tachycardia (116), and tachypnoea (26), which together suggest possible infection. Combined with the patient’s recent surgery, I’m concerned about post-operative infection or sepsis developing. I would escalate urgently to the medical team for assessment and investigations.”
Shift 2: Contextual Assessment Over Algorithmic Response
Examiners now expect you to ask and consider:
- What is this patient’s baseline? (A post-op patient with elevated RR day 1 is expected)
- What is their reason for admission?
- What are their chronic conditions? (COPD, diabetes, heart failure)
- Has there been a change in observations? (Change is always concerning)
Practical implication: Before escalating, consider context. Say: “Patient is post-operative day 2. Mild elevation in RR and pulse is expected. However, combined with fever and lower SpO₂, this warrants escalation to rule out post-operative complications like infection.”
Shift 3: Communication of Clinical Risk
The 2026 framework prioritises your ability to communicate escalation concerns clearly to colleagues.
When you escalate, don’t just call and say, “NEWS2 is 6.” Instead, give a structured handover. For example:
“Hi, I’m calling about Mr. Singh in bed 7. He’s day 2 post-op following abdominal surgery. His NEWS2 is 6, and I’m particularly concerned about his fever (39.2°C), elevated respiratory rate (28), low SpO₂ (91%), and tachycardia (106). This pattern is concerning for possible post-operative infection or sepsis. He’s alert but appears unwell. Can you come and assess him urgently?”
This is what examiners listen for in 2026 OSCE-clear, concise, clinically reasoned communication.
Real OSCE Scenarios: Complete Assessments Showing NEWS2 in Context
Seeing NEWS2 integrated into full clinical assessments is crucial. Here are three realistic scenarios at different complexity levels:
Scenario 1: The Stable Pre-Operative Patient (NEWS2 = 0)
The situation: You’re assessing Mr. Ahmed, a 55-year-old admitted for elective knee replacement surgery tomorrow. There are no acute concerns.
Vital signs recorded:
- RR: 16 breaths/min → Score 0
- SpO₂: 98% on room air → Score 0
- Systolic BP: 140 mmHg → Score 0
- Pulse: 78 bpm → Score 0
- Consciousness: Alert and orientated × 3 → Score 0
- Temperature: 36.8°C → Score 0
- Total NEWS2 = 0
What you say in OSCE:
“Mr. Ahmed’s observations are all within normal limits. Total NEWS2 is 0. This patient is stable and ready for surgery tomorrow. I would continue routine pre-operative observations 12-hourly, ensure he’s compliant with pre-operative fasting guidelines, and document that there are no acute concerns. I would also confirm he’s received pre-operative education and is psychologically prepared for surgery.”
What examiners are thinking: Accurate recording, correct scoring, appropriate interpretation, clear communication, professional approach.
Where this fits in broader OSCE: This is your baseline. Examiners want to see you can accurately assess stable patients, not just focus on deteriorating ones.
Scenario 2: The Borderline Patient With Early Signs of Infection (NEWS2 = 4)
The situation: Mrs. Patel is a 68-year-old admitted 2 days ago with a urinary tract infection. Her daughter called the bell because she seems less responsive than yesterday.
Vital signs recorded:
- RR: 22 breaths/min → Score 1 (range 21-24)
- SpO₂: 94% on room air → Score 1 (range 93-94)
- Systolic BP: 155 mmHg → Score 0 (range 90-180)
- Pulse: 104 bpm → Score 1 (range 101-110)
- Consciousness: Alert but drowsy → Score 0 (Alert still, but trending toward concern)
- Temperature: 38.2°C → Score 1 (range 37.6-38.4)
- Total NEWS2 = 4
What you say in OSCE:
“Mrs. Patel’s NEWS2 is 4. She has fever, slightly elevated respiratory rate, lower oxygen saturation, and tachycardia-a pattern consistent with active infection. Additionally, I’m concerned that she’s drowsier than yesterday, which could indicate early sepsis progression. While a NEWS2 of 4 is in the amber zone, the combination of fever and altered responsiveness warrants escalation. I would inform the nurse-in-charge immediately and increase observations to 4-6 hourly. I would also recommend the medical team assess her for possible urosepsis and consider investigations like blood cultures, urinalysis, and chest X-ray. I would ensure she’s adequately hydrated and monitor closely for further deterioration.”
What examiners are thinking: You’ve recognised a pattern (infection + change in consciousness = possible progression). You’ve escalated appropriately. You’ve considered what investigations might be needed. This is clinical reasoning.
Link to related skill: This scenario relates to Why Reading the NMC OSCE Scenario Is Crucial for Exam Success-you read that she’s “less responsive than yesterday,” which is the critical contextual clue that triggered escalation beyond the raw NEWS2 number.
Scenario 3: The Deteriorating Post-Operative Patient (NEWS2 = 8-Emergency)
The situation: Mr. Singh is a 70-year-old post-operative patient (day 2 following abdominal surgery). He’s been complaining of feeling “unwell” all morning. You respond to his call bell.
Vital signs recorded:
- RR: 28 breaths/min → Score 2 (range 25-30)
- SpO₂: 89% on room air → Score 3 (<91)
- Systolic BP: 85 mmHg → Score 2 (range 71-80)
- Pulse: 120 bpm → Score 2 (range 111-130)
- Consciousness: Alert but anxious → Score 0
- Temperature: 39.4°C → Score 3 (>39)
- Total NEWS2 = 2 + 3 + 2 + 2 + 0 + 3 = 12
What you say in OSCE:
“Mr. Singh’s NEWS2 is 12. This is a medical emergency. He has multiple critical red flags: severe hypoxaemia (SpO₂ 89%), high fever (39.4°C), tachycardia (120), tachypnoea (28), and hypotension (85 mmHg). Additionally, he has two parameters scoring 3 (SpO₂ and temperature), which mandates immediate escalation. This pattern is highly concerning for sepsis, possibly from wound infection or intra-abdominal infection post-operatively.
I would immediately:
- Call for emergency medical team assessment right now-not in a few minutes
- Stay with the patient and implement continuous monitoring
- Ensure IV access is established and prepare for possible fluid resuscitation
- Consider oxygen therapy escalation-he needs higher-flow oxygen urgently
- Alert the surgical team given his post-operative status
- Prepare for possible ICU admission
- Document clearly: time, observations, escalation action, clinical reasoning
While waiting for the team, I would talk to Mr. Singh: ‘You’ve developed signs that need urgent attention from the doctors. I’m getting them here right now. I’m staying with you and we’re going to make sure you get the care you need.'”
What examiners are thinking: You recognised the emergency. You escalated immediately (no hesitation). You demonstrated the pattern recognition (post-op + fever + hypotension + hypoxaemia = possible sepsis). You communicated with both the team and the patient. You stayed calm while acting with urgency. This is what passing OSCE looks like.
Link to related skills: This scenario draws on multiple competencies:
- Red Flags in the NMC OSCE: What Every Candidate Must Know-you identified the red flags (hypotension, hypoxaemia, fever)
- Common Errors in the NMC OSCE Silent Clinical Skills-you avoided the error of hesitation or underestimating severity
- A Clinical Approach to Neurological Assessment-you noted his altered mental state (anxiety could indicate cerebral hypoxia)
Frequently Asked Questions: What Every Nurse Wonders About NEWS2 in OSCE
Q: What if I miscount vital signs? Does the examiner stop me?
A: The examiner won’t stop you mid-procedure. However, they will note inaccuracies. If you’re unsure about a vital sign reading, it’s acceptable to retake it-this shows attention to detail, not incompetence. Say, “Let me recheck that-I want to be accurate,” and retake the measurement.
Q: Is NEWS2 always the same, or do different hospitals use different versions?
A: NEWS2 is standardised nationally and internationally. The scoring ranges you’re practicing with in 2026 are the same across all NHS trusts. Some hospitals may have local escalation protocols (e.g., “Call outreach at NEWS2 ≥5”), but the NEWS2 calculation itself is uniform.
Q: How do I explain NEWS2 to a patient in OSCE?
A: This is a 2026 expectation-person-centred care means explaining what you’re doing. You might say: “I’m going to check your vital signs-that’s your temperature, blood pressure, heart rate, breathing, and oxygen level. These measurements help me understand how your body is coping with your condition. It’s routine and takes about 5 minutes. Is that okay?” Keep it simple and reassuring.
Q: If NEWS2 is 0, do I still document it completely?
A: Absolutely. Documentation is crucial even when observations are normal. Examiners assess: (a) accurate recording, (b) correct scoring, (c) clear documentation. A patient with all normal vital signs still needs the chart completed fully and signed.
Q: Can I use a calculator or app to compute NEWS2 in OSCE?
A: No. You’ll calculate manually using the chart. Practice mental math so you’re fast and accurate. Being able to quickly interpret NEWS2 and explain it demonstrates competence to examiners.
Q: How does NEWS2 relate to other assessment stations?
A: NEWS2 is primarily tested in Assessment Stations, but you may reference it in other stations. For example:
- In Master the A-E Assessment of NMC OSCE Assessment Station, NEWS2 interpretation is part of the “Circulation” component
- In Red Flags in the NMC OSCE, elevated NEWS2 scores are red flags
- In MUST Score Management Guide, NEWS2 is one tool among several assessment frameworks
- In How to Master NMC OSCE Assessment Station in Community and Hospital Settings, NEWS2 anchors the vital signs assessment
Q: What if the patient refuses to have observations taken?
A: In OSCE with a patient actor, this won’t happen. However, in your verbalisation, show you’d respect autonomy: “If a patient refused observations, I would explain why vital signs are important for their safety. If they still refused, I would document this and escalate to the nurse-in-charge for discussion about capacity and consent.”
Q: What if I disagree with my NEWS2 calculation? Can I change it?
A: If you’ve calculated NEWS2 and the examiner questions it, explain your reasoning calmly: “I scored respiration rate as 1 because it’s 22, which falls in the range 21-24. Is my interpretation different from yours?” This opens dialogue. If you genuinely made an error, it’s better to recognise it: “Actually, let me recheck that. Temperature 38.4 falls in the Score 1 range, not Score 2. My total should be [recalculated].” Examiners respect self-correction.
Your Quick Reference Guide: NEWS2 Scores and Actions at a Glance
Use this summary when you’re under exam pressure:
NEWS2 = 0 (Green Light)
→ Patient is stable
→ Continue routine 12-hourly monitoring
→ Document observations clearly
→ No escalation needed
NEWS2 = 1-4 (Amber Light)
→ Patient has some abnormalities
→ Inform nurse-in-charge
→ Increase observations to 4-6 hourly
→ Assess for other clinical concerns
→ Escalate if condition worsens or new symptoms develop
NEWS2 = 5-6 OR Any Parameter = 3 (Orange Light)
→ Escalate immediately to medical team
→ Increase monitoring to hourly
→ Prepare for possible critical care referral
→ Document clearly and communicate clinical concerns
→ Stay alert for further deterioration
NEWS2 ≥ 7 (Red Light-Emergency)
→ This is a medical emergency
→ Call for immediate senior clinician assessment
→ Activate critical care involvement
→ Implement continuous monitoring
→ Prepare for possible ICU admission
→ Ensure IV access and oxygen delivery optimised
How NEWS2 Connects to Your Broader OSCE Preparation and Success
Mastering NEWS2 is one critical pillar of Assessment Station excellence. Here are the complementary knowledge areas and skills that together form a complete assessment station competency:
Core assessment skills related to NEWS2:
- Why Reading the NMC OSCE Scenario Is Crucial for Exam Success
- Context shapes interpretation. Before you record a single vital sign, understand the patient’s history, reason for admission, and baseline.
- Common Errors in the NMC OSCE Silent Clinical Skills
- Silent station mistakes (like inaccurate vital signs) cascade into NEWS2 errors. Master the technical skills first.
- A Clinical Approach to Neurological Assessment in the NMC OSCE
- Consciousness level (part of NEWS2) connects to neurological deterioration. Understanding GCS helps refine your AVPU assessment.
- Red Flags in the NMC OSCE: What Every Candidate Must Know
- Red flags often correlate with elevated NEWS2 scores. Learn to recognise patterns (fever + cough + tachypnoea = respiratory infection).
- 6 Tips to Answer in NMC OSCE Scenario Based Nursing Problems
- NEWS2 interpretation helps you identify nursing diagnoses and prioritise interventions.
- MUST Score Management Guide for NMC OSCE Success
- NEWS2 is one assessment framework. The MUST (Malnutrition Universal Screening Tool) is another. Understanding both together strengthens your assessment station performance.
- How to Master NMC OSCE Assessment Station in Community and Hospital Settings
- The complete Assessment Station guide covering vital signs, NEWS2, documentation, and escalation in both community and hospital contexts.
- What to Expect on Your NMC OSCE Exam Day
- Understanding the exam structure helps you mentally prepare for NEWS2 scenarios and time management.
Final Insights: Why NEWS2 Mastery Matters Beyond OSCE
NEWS2 isn’t just an OSCE test. It’s a real clinical tool you’ll use every shift as a UK registered nurse. Every day, you’ll take observations and calculate NEWS2 to guide patient safety decisions. Patients’ safety depends on your accuracy and clinical reasoning.
In your OSCE exam, examiners are assessing not just whether you can calculate NEWS2, but whether you understand why it matters:
- Can you recognise deterioration early?
- Can you escalate appropriately without hesitation?
- Can you communicate clinical risk clearly to colleagues?
- Can you provide person-centred care while managing emergencies?
Master NEWS2 now, and you’re not just passing OSCE-you’re building the foundation for safe, confident nursing practice as a UK registered nurse.
Enhance Your NMC OSCE Preparation
Our comprehensive OSCE training is designed to help you excel in the NMC OSCE exam. With tailored guidance, practice scenarios, and expert support, we ensure you’re fully equipped with the skills and confidence to succeed. Sign up for our OSCE course today and take your preparation to the next level! Also, check out the guide to prepare for NMC OSCE.
NMC OSCE For nurses Everything You Need to Know in 2024 👉 Click Here
For Any NMC OSCE Related Queries and Training Chat with Us!